Islet Cell Transplantation Research Highlights
Increasing Islet Supply
Islet cell transplantation is limited by the amount of donor tissue available. If islet cell transplantation is to one day become a widespread treatment for diabetes, additional sources of islet cells will likely be necessary to treat all patients. City of Hope scientists are working to address this problem by differentiating embryonic stem cells or adult progenitor cells from the pancreas into insulin-producing cells. Once perfected, such strategies could potentially make available an unlimited supply of islets for transplant.
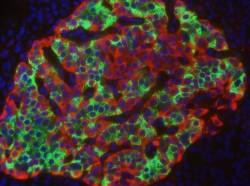
Islet Imaging
It is difficult to monitor islets after their transplantation into the liver. The ability to image transplanted islets would be an important way to monitor their survival. Scientists at City of Hope are developing an innovative approach to image transplanted islets as well as, islets in the native pancreas. This approach will allow islets to be visualized using currently available medical equipment (e.g., MRI, PET). The technique is expected to provide safe, effective and high quality images for repeatable monitoring of islets after transplantation into the liver or to detect islet survival in newly diagnosed diabetic patients. Having a reliable means of visualizing islet health within the body would provide further opportunity for interventions to protect the cells when abnormalities are detected. This research is funded by the JDRF.
Islet Gene Profiling
Scientists at City of Hope and Scripps Institute are also exploring ways to evaluate islet health and survival with genetic testing. By evaluating the genes present in high-quality versus low-quality islet preparations, it may be possible to identify important gene markers that will allow scientists to screen islets for health and functionality prior to transplant. It may also be possible to test for islet gene markers in the blood of patients with diabetes or in those who have received an islet transplant to monitor cell survival. This research is partially funded by the Juvenile Diabetes Research Foundation.
Immune Tolerance
Islet transplantation currently requires patients to take powerful immunosuppression medications for the rest of their lives to prevent destruction of the transplanted islet tissue by the immune system. Immunosuppression medications are associated with a number of health risks such as increased risk of infection and other potentially debilitating side effects, and as a result, islet transplantation is currently only permitted in patients with severe forms of type 1 diabetes.
City of Hope scientists are developing alternative strategies to prevent the immune system from rejecting islet cells without the need for immunosuppression medications by establishing mixed chimerism (coexistence of donor and recipient cells), using bone marrow stem cells and regulatory T cells. The development of these “immune tolerance” strategies would reduce the risks of the islet transplant procedure and improve islet transplant outcomes making it an appropriate treatment for more patients with diabetes.