Myeloma
March 13, 2024
This page was reviewed under our medical and editorial policy by Michael Rosenzweig, M.D., Chief, Division of Multiple Myeloma, City of Hope Duarte
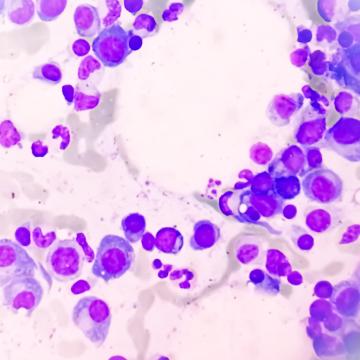
Myeloma, also called multiple myeloma, is a type of blood cancer that develops when plasma cells — infection-fighting blood cells in the immune system — become abnormal and grow and divide uncontrollably to become tumors.
These tumors then crowd out normal blood cells in the patient's bone marrow, weakening the immune system. This may make the patient more susceptible to an infection. The cancerous cells may also travel through the patient's bloodstream and affect bones throughout the body.
Myeloma is a relatively rare cancer — accounting for an estimated 1.8% of all new cancer cases in the United States. The most significant risk factor for developing myeloma is older age, and this type of cancer rarely affects patients over the age of 45.
Myeloma doesn’t always cause symptoms. That’s why some cases are only discovered after blood or urine tests yield abnormal results. When symptoms do occur, they may include bone pain, unexplained fevers, easy bruising or bleeding, fatigue, weakness and frequent infections
If a myeloma diagnosis is suspected, the care team will perform a series of tests, which may include blood and urine tests, bone marrow aspiration and biopsy, imaging studies and genetic tests.
When a patient receives a myeloma diagnosis, the care team may tell them they have a specific type of the disease. Treatments are then customized to that type of cancer, as well as the patient’s goals and overall health. The types of disease include smoldering, light chain, extramedullary, active myeloma and solitary plasmacytoma, among others.
Myeloma treatment plans are individualized to each patient's specific needs and disease stage. Options may include chemotherapy, immunotherapy, radiation therapy, stem cell or bone marrow transplantation, CAR T-cell therapy, targeted therapy and more.
Getting treated for myeloma at City of Hope means you are steps away from labs where new cancer treatments are being developed every day. That proximity means you benefit from something unique in cancer care — “bench-to-bedside” treatment.
When you come to City of Hope, you have access to a strong network of support services and staff to help you and your family along your myeloma journey.
Patient Stories

City of Hope is among a dozen national centers that treat myeloma with a multidisciplinary team solely focused on this type of cancer.
A National Cancer Institute-designated comprehensive cancer center, City of Hope has been named one of America's top cancer hospitals by U.S. News & World Report for over a decade. Through our cancer experts in Duarte, California, as well as Phoenix, Chicago and Atlanta, our blood cancer experts offer leading-edge care and treatments for myeloma.
Our Myeloma Program Highlights
City of Hope's myeloma program is staffed with experts who provide leading-edge care and perform innovative research to better understand the disease and to tailor each patient's treatment to his or her goals and myeloma type. Below are a few of the highlights of this program.
- The Judy and Bernard Briskin Center for Multiple Myeloma Research within the Hematologic Malignancies Research Institute is among the largest programs of its kind in California, treating hundreds of new myeloma patients every year. It leads the development of a diverse portfolio of over 15 active phase 1 and 2 clinical trials for all multiple myeloma stages.
- The center aims to make multiple myeloma and related light-chain amyloidosis manageable and nonlethal through immunotherapy and rational combinatorial therapies.
- It aggressively pursues research on improved treatments and collaborates with myeloma and amyloid experts nationally and internationally.
- City of Hope offers promising therapies, like gene, CAR T-cell and antibody, that boost the immune system's cancer-fighting response as part of the Kenneth Goldman and Briskin Family Clinical Trials Program.
- Our experts have unrivaled immunotherapy expertise — including involvement in groundbreaking early drug trials like for daratumumab, the first monoclonal antibody approved for successful myeloma treatment.
- We collaborate with the Multiple Myeloma Research Consortium.
- City of Hope is home to one of the most prominent U.S. blood and bone marrow transplant centers. Its innovative approaches include combining transplantation with new therapies.
- We understand unique issues for older patients and use computer models to predict toxicity and tailor treatments for efficacy and fewer side effects.
- Our highly trained, experienced nurses offer outpatient support for bone marrow transplant patients.
- We customize genetic testing and drug therapy to the molecular profile of specific myeloma types.
Each myeloma patient's care includes regular interaction and input from hematologists, oncologists, radiologists and pathologists, nurses, social workers, and specially trained support staff. This team brings together deep experience and diverse perspectives to arrive at the ideal treatment for each patient. Throughout and following treatment, patients are supported and monitored by our survivorship clinics.

Advancements and current innovative treatment approaches have resulted in myeloma survival rates at City of Hope that exceed the SEER National median survival for multiple myeloma.

Our developments in the areas of breakthrough cancer drugs, bone marrow transplants and CAR T cell therapy are recognized internationally.
Our leadership in research and innovation continually enhances our ability to provide novel and differentiated approaches to cancer care.
Azra Borogovac, M.D., M.S., is a hematologist at City of Hope Orange County Lennar Foundation Cancer Center. For Dr. Borogovac, the patient is the most important part of the medical team. She sees the opportunity to provide care to people with cancer as a privilege.

Scott Goldsmith, M.D., specializes in the treatment of multiple myeloma, which is also the focus of his prolific research.
Maung Myo Htut, M.D., is determined to find more effective treatments for multiple myeloma, a rare blood cancer that strikes about 30,000 Americans each year. He believes the body's own immune system may hold the key.

Murali Janakiram, M.D., M.S., is a hematologist-oncologist and associate professor in the department of Hematology and Hematopoietic Cell Transplantation.

Amrita Krishnan, M.D., directs the Judy and Bernard Briskin Center for Multiple Myeloma Research at City of Hope's cancer research hospital, seeking to make gains in one of the most rapidly changing areas in cancer research.
Sarah S. Lee, M.D., is an assistant clinical professor in the Department of Hematology & Hematopoietic Cell Transplantation, who studies precision therapy for plasma cell disorders like multiple myeloma and amyloidosis.
Nitya Nathwani, M.D., is an associate professor in Hematology & Hematopoietic Cell Transplantation and a hematologist/oncologist at City of Hope in Los Angeles, California.

Michael Rosenzweig, M.D., is Chief, Division of Multiple Myeloma and a hematologist-oncologist, in the Department of Hematology & Hematopoietic Cell Transplantation at City of Hope in Duarte, CA.

Flavia Pichiorri, Ph.D., M.S., is a professor in the Department of Hematologic Malignancies Translational Science.
Dr. Wang is a molecular epidemiologist whose multifaceted research spans the evaluation of genes and heritability, the physical and social environment, and their interactions in cancer and cardiovascular disease etiologies, leveraging data from large cohort and international consortia.
Multiple Myeloma Research Foundation. Understanding Multiple Myeloma.
https://themmrf.org/multiple-myeloma/American Cancer Society (2024, January 19). Key Statistics About Multiple Myeloma.
https://www.cancer.org/cancer/types/multiple-myeloma/about/key-statistics.htmNational Cancer Institute (2024). Myeloma Stat Facts.
https://seer.cancer.gov/statfacts/html/mulmy.html