Larry Jarvis knows all about tough challenges.
For 33 years, he served proudly in the Los Angeles Fire Department, rising to the rank of captain. He remembers more than a few dicey situations, like battling seemingly endless fires touched off by warring gangs. He recalls fertilizer blazes that filled the sky with purple, green and yellow smoke and spewed noxious fumes. And more.
None of it fazed him. He and his wife Petra both understood that firefighting can be hazardous to one’s health.
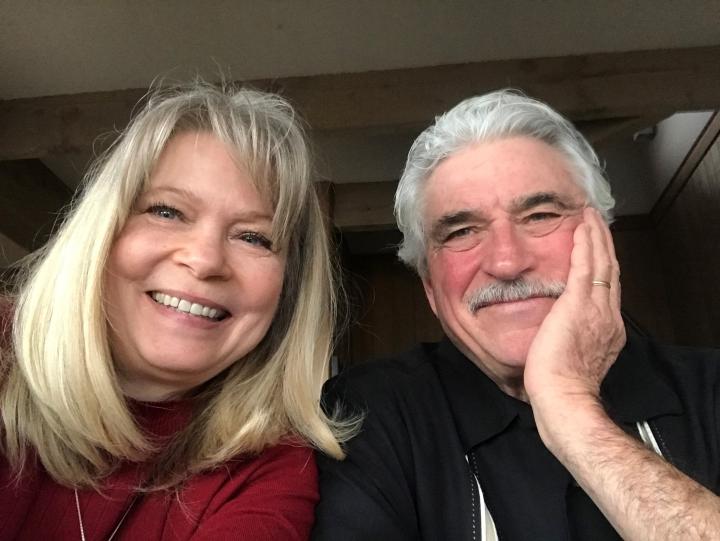
“We talked about it before we got married,” said Petra. “We were told that being a firefighter took 10 years off your life. But we were young and in love, and those were just statistics. We had concerns, but never fear.”
Another grim fact: For many years, heart disease was the No. 1 killer of firefighters. It no longer is. Cancer has replaced it.
Those statistics didn’t deter Larry from entering the field in his early 20s. He wanted to serve, and he saw firefighting as the perfect way to use his athletic abilities to help others.
“There’s a sense of purpose,” he said. “A feeling that I’ve contributed. I’ve done good.”
Treated at City of Hope 15 Years Ago
In 2007, when he was 58, Larry was treated successfully at City of Hope for prostate cancer. When he retired in 2010, his health was fine and he and Petra looked forward to a happy future, dividing their time between their homes in Bellingham, Washington, and Santa Clarita, California, traveling (including biking through France), enjoying their children and grandchildren, and just having more time for each other. “Our goal,” said Petra, “was to enjoy retirement and our time together.”
The plan worked well for more than a decade. But in June 2021, at the age of 72, Larry began to rapidly lose weight (“40 pounds in two months!” he recalled, “I looked like a 144-pound glow stick!”). When he woke up one morning with jaundice, he knew something serious had happened. And he knew what he had to do next.
“There was no question where I would go,” he recalled. Larry reconnected with the City of Hope doctors who had treated his prostate cancer years earlier. They immediately ferried him to the proper department. Within two days, Larry was meeting with oncologist Vincent Chung, M.D., who delivered the ominous diagnosis: Stage 4 pancreatic cancer.
“We knew that pancreatic cancer was generally considered not as ‘hopeful’ as other cancers,” said Petra, putting it about as mildly as one can. Each year, pancreatic cancer strikes some 64,000 people in the U.S. and claims more than 50,000.
Pancreatic cancer is difficult to detect in its early stages because symptoms generally don’t appear until the cancer has grown and spread.
As a result, the prognosis is usually grim. If the cancer hasn’t spread and can be surgically removed, the five-year survival rate is 42%. But only about 13% of people are lucky enough to be diagnosed so early. If the cancer has spread to surrounding tissues or organs, the five-year survival rate drops to 14%. By the time the cancer advances to Stage 4 — Larry’s situation — the five-year survival rate is a paltry 1%. Most of those patients don’t survive longer than one year.
No one knows what causes pancreatic cancer, but there are risk factors. Smoking is one. Another is exposure to workplace chemicals. One possible culprit may be AFFF: the Aqueous Film Forming Foam often used by firefighters. Chemicals known as PFAS (per- and polyfluoroalkyl substances) in the foam have been linked to a dozen different malignancies, including pancreatic cancer. Larry was quite familiar with the material.
“We used it. We trained with it. We stored it. We were always around it,” he said.
Supported by their deep faith, Larry and Petra agreed they would give this battle everything they had.
“I was ready for a fight,” said Larry. “I knew we had the best team. It was a situation that God put me in for a purpose. So, I was going to be positive and fight as hard as I can.”
“I felt there were three options,” added Petra. “Do nothing. Panic. Or get to work.” She says it’s in her nature to “buckle down” when faced with a tough challenge.
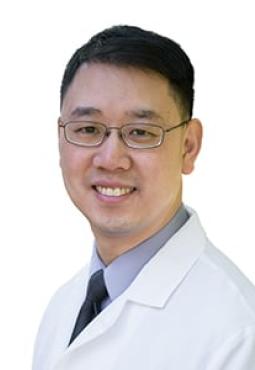
'We have a plan that works very well. Patients can keep their ‘treatment’ physician in Duarte, but they can also get a "local" physician.'
George Hajjar, M.D.
Most Stage 4 patients receive chemotherapy. But in Larry’s case, he first needed intestinal bypass surgery because the tumor was blocking his digestive system. Once recovered, Larry began an aggressive regimen of oxaliplatin, fluorouracil and irinotecan, three of the most common chemotherapy drugs for pancreatic cancer. Larry lost his hair and experienced some neuropathy, but by and large he handled the treatment well.

The Jarvises loved their care team at City of Hope. The biweekly, three-hour commute, not so much. Happily, Larry was able to seamlessly transfer his treatment to City of Hope’s Santa Clarita clinical network site, an 8,500-square-foot facility lined with picture windows overlooking lush landscaping (patients call it “The Treehouse”) and staffed by a dozen medical and surgical oncologists with a full complement of medical, laboratory and diagnostic radiology services. And all of it just a 10-minute drive from his home.
Medical oncologist George Hajjar, M.D., City of Hope’s regional medical director for the San Fernando Valley and Ventura County, picked up Larry’s care in Santa Clarita without missing a beat. Continuity of care was scrupulously maintained.
“We have a plan that works very well,” explained Hajjar. “Patients can keep their ‘treatment’ physician in Duarte, but they can also get a ‘local’ physician. So, patients who want to be treated close to home can do it.”
By the time Larry walked into Hajjar’s office for the first time, everything had been laid out in advance with an efficiency that impressed.
“He had all my information,” Larry said, admiringly. “My charts … he knew everything about my background and my treatment. From the very beginning, I felt comforted by his knowledge of who I was, and my goal to survive.”
Also comforting was the supportive atmosphere that greeted the Jarvises.
“People are so kind,” continued Larry. “Always asking how you’re feeling, always offering snacks, always checking every little thing.”
“What a blessing to have that place so close to home,” agreed Petra, “and to feel so confident that the good care would continue. I even like the brownies in the cafeteria! Real food, not hospital food. And Hajjar, he really listens. He’s so genuine and personable. He’s the cherry on top!”
Whether it’s the brownies, the smiles all around or the adept administration of powerful chemo, Larry has so far beaten the odds. Nearly two years in, his cancer, though not eradicated, is under control. His CA-19-9 levels (a tumor marker for pancreatic cancer), once as high as 7,600, are below 100 now (a normal level is about 30). He understands that things may change, and he is prepared to face that as well, perhaps moving on to newer immunotherapy treatments.
“He’s such a blessed man,” said Hajjar of the patient who has also become his friend. “He’s doing better than expected, responding well and having minimal side effects.”
“I feel good,” agrees Larry. There are many days, he says, when he hardly remembers he has cancer at all … and other days, to be sure, when fatigue and flu-like systems drift in. He’s handling it, even signing up to speak on behalf of City of Hope and share his experiences at pancreatic cancer support groups.
“We’re hopeful about the future,” said Petra. “And we have the proper team around us.
“We’re so thankful.”
