It isn’t often that you find both a hero and a medical pioneer in the same family. But such is the case with teen sisters Leen and Jana Faytrouni of Riverside, California.
They were always close, doing things together all the time — baking is a favorite activity. But for a few years now they have shared a unique bond that saved Leen’s life while helping to advance leukemia research and treatment.
“It’s a miracle, all we’ve been through,” said their father Omar Faytrouni, an IT networking specialist originally from Lebanon. “It’s a blessing.”
In mid-2020, Leen, who was 12 at the time, stopped being the normal, healthy, active kid she had always been.
“I was getting tired, running out of breath,” she recalled, “I couldn’t eat the way I used to, and I was running a fever for no reason.”
Mom noticed. Also from Lebanon, Racha Faytrouni is a science teacher and a passionate researcher who, according to her husband, “knows as much as many nurses.”
“She was really pale, not as energetic as she used to be,” said Racha. “I thought perhaps it was because we were fasting during Ramadan. But she was also getting nosebleeds, bloody gums. I thought it might be leukemia. I had read about it.”
Despite the COVID-19 lockdown and those early fears of visiting a doctor’s office, Leen’s parents brought her in for blood tests.
Alarm bells went off quickly. Leen’s pediatrician wanted more tests. When the results came in, the news was overwhelming.
“My wife came to me crying,” said Omar.
“I’ll never forget the date: July 7, 2020,” said Racha. “I was in the middle of teaching an online class. I had to stop. I felt terrible. I’m holding Omar and saying, ‘Oh, she’s going to suffer! It’s not going to be easy for all of us!’”
Dad tried to stay positive — but indeed, it wasn’t easy.
“I come from a religious background, so I’m thinking thank God, we’ll work around this, take whatever steps are necessary,” he said. “But it’s hard for a dad to see this happen to his first baby.”
Teen’s AML Diagnosis
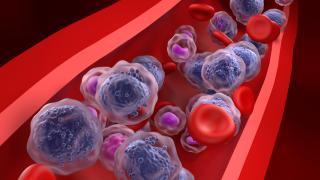
Leen was diagnosed with acute myeloid leukemia (AML), a blood cancer more common in adults. AML strikes only about 500 children each year, and Leen’s case was particularly rare. She was found to have a “mixed lineage” variety of the disease, in which rearrangements occur in the MLL gene, making this form of leukemia even more aggressive and tougher to treat.
Her doctors mapped out a plan involving five cycles of chemotherapy, anchored by the drug cytarabine, which interferes with cancer cells’ DNA replication.
Most children with leukemia respond well to chemotherapy and, for a while, so did Leen. She bravely endured the typical side effects: nausea, fatigue and hair loss. Happily, after each of the first four cycles, a biopsy showed no sign of cancer. Leen excitedly planned her imminent release from the hospital, buying new furniture for her bedroom and looking forward to returning to her normal life.
But two weeks after cycle five, that optimistic mood vanished. The last biopsy revealed her leukemia had returned.
“I was really sad,” Leen remembered. “It felt like all that treatment had gone to waste. And I didn’t want to go back to the hospital.”
But she did go back, for an additional two cycles of different chemotherapy regimens. Neither worked. Leen was running out of options. Even a stem cell transplant seemed out of the question because nothing seemed capable of putting Leen into remission, an essential step before a transplant can be done.
Revumenib Trial Leads to Remission
But timing, they say, is everything.
“We were home, waiting for something to happen,” said Racha. “I was devastated. But then we got a call from our doctor, who told us about a clinical trial at City of Hope.”
It turns out that City of Hope researchers had been investigating a drug called revumenib, a so-called “menin inhibitor.” When the menin protein interacts with the altered MLL gene, normal blood cell development is disrupted. These underdeveloped cells proliferate and crowd out the healthy cells, causing aggressive leukemia. The thinking was that blocking menin’s action could allow normal, healthy blood cells to grow.
The early data was promising. Revumenib helped many patients achieve complete remission, enabling several to receive successful transplants. But those patients were adults. Would revumenib work as well in children? City of Hope aimed to find out, and Leen would be their first attempt.

“They were very scared, but Leen was very stoic,” said Nicole A. Karras, M.D., a pediatric hematologist-oncologist and associate clinical professor in City of Hope’s Children’s Cancer Center, recalling her first meeting with the family, during which she explained the clinical trial. “There was a lot of learning for everybody. Obviously, they were worried. But they didn’t have a lot of choices.”
They didn’t need much convincing. “I researched it,” said Racha, “and I felt good about it.”
Revumenib, taken in pill form, works quickly and without chemo’s toxicity. Leen tolerated the drug well and went into remission as predicted. “Those were our best days in months,” recalled Omar. “No pain, no side effects. It was a big blessing.”
Nevertheless, because this particular form of aggressive leukemia could very likely recur, the family now began preparations for Leen to get a transplant. They launched a bone marrow drive through the Be The Match organization to find a donor. Three were located in different parts of the world, but none was available. After testing family members, Karras decided that Leen’s younger sister Jana (9 at the time) would be the best match. “We like younger donors,” said Karras. “They have more stem cells.”
Jana needed a bit of persuading, but eventually stepped up heroically.
“I was scared at first. I didn’t want to do it,” she remembered. “But when I realized it could get rid of the cancer, I felt like I had to, and then I wanted to.”
Imagine the emotions flowing through the girls’ parents who had never left Leen’s side, every day of her previous hospitalizations. The only exception was when Mom and Dad both came down with COVID-19, a very difficult time for all.
And now here was Jana in one hospital room, preparing to donate her bone marrow. And down the hall, Leen waited in another room (COVID-19 and hospital protocols didn’t allow them to be together).
“Racha and I split our time on that floor, going back and forth to each room,” Omar said.
It was a bumpy road at first for Leen. The intense chemotherapy required for several weeks pretransplant caused bloating, pain, fatigue, loss of appetite and more. “At one point I just said, ‘I don’t want to live,’” she remembered. Fortunately, the worst symptoms cleared up after a few days.
Managing Graft-Versus-Host-Disease
The transplant took place in September 2021. Leen experienced trouble afterward: a liver blockage and temporary kidney failure requiring dialysis. Her City of Hope team dealt with all of it, along with a mild case of graft-versus-host disease.
City of Hope’s supportive care services team also pitched in, finding a nearby apartment for Racha and Omar so they wouldn’t have to commute daily from their Riverside home while Leen was hospitalized. Leen benefited from visits by a psychologist, as well as sessions with an occupational therapist. Child life specialist Megan Matthews did craft projects with her. And the whole family marveled at the volume of donated gift cards, gift baskets and other goodies they received from City of Hope at Christmastime and on Leen’s birthday.
And the sisters finally got to see each other. They got special permission to spend one night in the same room, watching a movie. “They have such a close bond now,” Omar said. “I see it. I feel it.”
By December 2021, Leen was well enough to go home, cancer free thanks to the transplant. She “rang the bell” signaling the end of her treatment, with her family and Karras looking on.
“Dr. Karras had tears in her eyes,” Racha remembered. “That made me cry, too. It showed how much she loves Leen, and all her patients.”
Today, Leen is thriving. Now in 11th grade, she completed middle school online while in the hospital (“with an A+ average!” her parents proudly point out). She still gets fatigued, and her cancer treatment may have affected her ability to have children — that is still unclear. But Leen’s OK with it. She’s thinking about a career as an anesthesiologist, fondly remembering the ones who helped her through multiple biopsies.
Meanwhile, City of Hope researchers made quite a splash when they presented the promising data on revumenib at the American Society of Hematology annual meeting in December 2023. The research, conducted at several sites across the U.S. and sponsored by drug company SNDX, showed that 63% of eligible patients had a positive response to the therapy, with 23% achieving complete remission.
The future for Leen? Karras is optimistic.
“We’re two years out now,” she said. “The longer we go, the less chance there is for a recurrence.”
The family is beyond grateful.
“Everyone at City of Hope was so nice,” said Omar. “It’s been an awesome experience from Day One.”
At City of Hope Children’s Cancer Center, our expert providers are dedicated to delivering world-class, personalized care for children, adolescents and young adults. Each patient is cared for by a multidisciplinary team of oncologists, hematologists, surgeons, radiation therapists, pathologists and supportive care staff, including child life specialists. Our team has access to leading-edge treatments, including our world-renowned stem cell and bone marrow transplantation programs and the latest clinical trials. Our specialists work together to develop a unique, targeted treatment plan for every patient while providing family support. Continuing care into adulthood for survivors, our Childhood, Adolescent and Young Adult Survivorship Program provides specialized follow-up care for patients who have completed treatment for cancer or a similar illness that was diagnosed before 40 years of age.