Radiation Therapy for Prostate Cancer
If radiation therapy is part of your prostate cancer treatment plan, it's a good idea to understand the options the care team may discuss with you.
External Beam Radiation Therapy (EBRT)
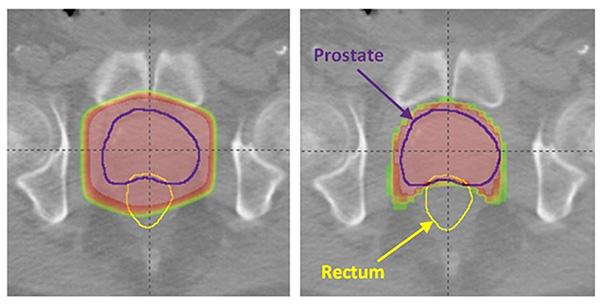
External beam radiation therapy uses radiation beams that are directed at the patient's tumor from outside the body to destroy cancer cells. EBRT is typically performed using either the TomoTherapy® or TrueBeam® machines. These image-guided radiation therapy treatments are typically delivered daily to reduce toxicity to the bowel, bladder and rectum. The care team will determine what is best for the patient to provide maximum radiation to the prostate cancer while reducing radiation to the nearby bladder, bowel and rectum. The picture below illustrates the benefit of TomoTherapy in sparing dosages to the rectum and bladder (on right) versus 3DCRT (on left).
Brachytherapy
With brachytherapy, also called internal radiation, the care team places radioactive material inside the patient's body so it can directly attack the tumor. The care team may perform a magnetic resonance imaging (MRI) scan of the prostate to better determine who may be a good candidate for brachytherapy.
MRI-Guided Ultrasound
MRI-guided focused ultrasound (MRGFUS) is an imaging treatment for prostate cancer that doesn't use radiation. Recently FDA-approved, focused ultrasound combines several capabilities that make it promising for cancer treatment.
First, the approach uses magnetic resonance to create a more precise image of the cancer so that treatment can be targeted specifically to the diseased area. The method then delivers focused ultrasound waves — heating up and destroying targeted areas of tissue inside the body without a single incision and avoiding healthy tissue. And it measures the temperature and energy accumulation at the treatment site in real-time, so that ultrasound waves can be highly controlled to ensure safety and effectiveness. In addition to providing more targeted, less invasive treatment, this approach offers new options to patients whose cancer has returned after traditional treatments have failed or who are too weak to withstand surgery or additional rounds of radiation.
City of Hope was the first institution in the United States to use focused ultrasound to treat prostate cancer. Unlike other forms of therapy such as surgery or radiation, only the portion of the prostate gland containing biopsy proven cancer is targeted with MRGFUS. Although still under investigation, this approach holds promise to reduce the risk of impotence and incontinence associated with other forms of prostate cancer therapy.
Post-Prostatectomy Radiation
Following prostatectomy, radiation therapy may be given post-operatively if certain features are seen in the pathology specimen. More commonly, radiation therapy is given for patients who show rises in the prostate-specific antigen (PSA) level during follow-up with their urologists. Patients are treated using image-guided, intensity-modulated radiation therapy (IG-IMRT) either on the TomoTherapy or TrueBeam machine.
The standard treatment lasts for approximately eight weeks, Monday-Friday. Harnessing the imaging platforms, patients typically receive an MRI in addition to traditional CT scanning for treatment planning. In some cases, the MRI may detect disease in the prostate bed that may otherwise have gone unnoticed, allowing the radiation oncologist to potentially give additional doses to these areas.
Clinical Trials Evaluating Radiation Therapy for Prostate Cancer
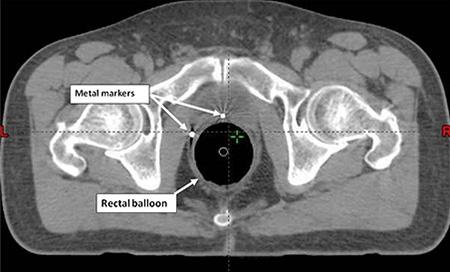
At City of Hope, we are enrolling patients for a groundbreaking clinical trial that is studying the safety and feasibility of using a shorter radiation treatment time to treat patients with rising PSA following prostatectomy. This is known as stereotactic body radiation therapy (SBRT). This technique utilizes IG-IMRT technology to deliver very focused and potent doses of radiation over one and a half weeks, and has been shown to be effective and safe in patients with prostate cancer who received radiation as their initial curative treatment. To assist in localization of the target, metal markers can be placed in the prostate bed under ultrasound guidance in the outpatient clinic. These markers will be detectable on the CT scans and be used to align the patient prior to each treatment delivery (see below image). Patients will also be evaluated for placement of a novel radiotransponder marker known as the Calypso® system. In addition, a rectal balloon will be inserted for the planning and daily treatments to ensure the target is stabilized, thereby maximizing the accuracy of treatment (also shown in the below image). Interested patients can contact City of Hope for further details regarding this study, and arrange for consultation.
Calypso System and Prostate Cancer

The care team may use a technology called the Calypso system, which involves placement of three beacon transponders (shown in the image) that will be tracked in real time by the Calypso technology. This allows the care team to track the movement of the prostate in real time and correct for interfraction movement for more precise imaging. Calypso recognizes the transponders via radiofrequency waves and can correct motion of as little as 2 millimeters (mm). For the patient, this means even more control with treating the prostate while sparing the nearby normal tissue such as the bladder and rectum.
Learn more about our radiation oncology or prostate cancer programs.