Radiation Therapy for Head and Neck Cancers Treatments
At City of Hope, we have been treating head and neck cancers using helical TomoTherapy since 2004, and therefore our department has extensive experience in planning and delivering such treatment.
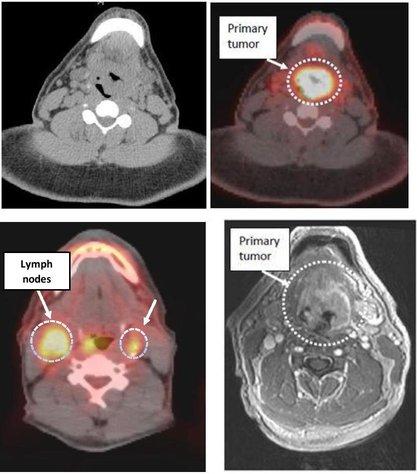
This technology combines radiation delivery with advanced imaging — including positron emission tomography (PET), magnetic resonance imaging (MRI) and three-dimensional computed tomography (CT) scans — so that treatment is precisely targeted to the tumor, while avoiding nearby normal tissues. Post-treatment imaging is also performed during follow-up appointments to ensure optimal outcomes for the patient.
Here is an example: The upper left figure shows a traditional CT scan of the neck used for treatment planning. The borders of the tumor are poorly outlined. With a fused PET/CT treatment planning scan (upper right figure), one can immediately recognize the boundaries of the tumor volume. The scan also demonstrated small lymph nodes in the neck with brightness levels consistent with tumor involvement (lower left figure). With CT alone, these lymph nodes would not have been covered in the high-dose treatment volume. Given the seamless PET/CT image fusion, it was possible to delineate these nodes in the treatment plan without distortion or uncertainty. Furthermore, with a fused MRI of the neck (lower right figure), additional information regarding tumor extension is now available. This data is easily incorporated into our planning.
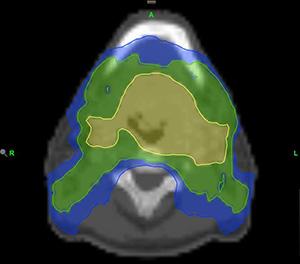
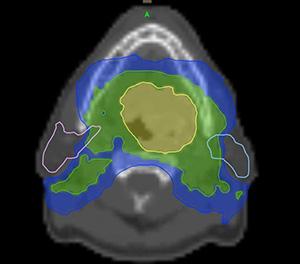
This figure shows the same patient’s TomoTherapy treatment plan: The color map displays different amounts of radiation dose being given to different areas within the head/neck. This is known as “dose-painting.” The distribution of radiation dose across the head/neck is customized to each patient’s individual tumor type and anatomy.
Radiation for Head AND Neck: What You Can Expect
If you’re having radiation therapy to the head and neck, this outline will help you prepare with information on what to expect before, during and after treatment.
Your treatment team will include:
- Radiation oncologist to plan your radiation therapy
- Radiation therapists to administer your radiation treatments
- Medical oncologist to provide chemotherapy
- Head and neck surgeons to remove, biopsy or evaluate cancer
- Nurses to manage your care
- Dentist to provide a preradiation dental evaluation and specialized care
- Swallowing specialist to teach you techniques to swallow, which can become difficult during treatment
- Dietician to help you chose the foods and liquids right for you
- Tobacco cessation specialist, if you smoke
Before treatment
Simulation
To be most effective, radiation therapy must be precisely targeted. Before beginning your treatment, you'll have a simulation — a treatment-planning procedure that recreates your anatomy and tumor in three dimensions, allowing for precise targeting and dose accuracy to the desired locations.
Preparing for your simulation:
- Follow any instructions your provider gives you regarding what to eat or drink.
- If you think you might be uncomfortable, bring Tylenol or another pain medication to take one hour before your procedure.
- Bring mouth guards if your dentist made them for you.
- Wear comfortable clothes.
- Remove earrings and necklaces.
During your simulation:
Your therapists will position you in the simulation machine. During the procedure, the table will move; lights will go on and off. Laser lights are used to guide you into the correct position — avoid looking directly into the beams. Therapists will explain what they're doing and talk you through the process. While someone will always be able to see and hear you, avoid speaking unless you need assistance as it can shift your position. Your therapists can play music for you or you can bring your own playlist.
- Positioning: Your provider will place you on a table in the simulation machine in the position you’ll hold during treatment. Immobilization devices such as molds and masks are customized to help you stay in the same position.
- Mask: To make your mask, your therapist will place wet plastic mesh over your face, shaping it around your head as you lie on the table. The mask will harden in about 15 minutes. During your simulation and treatment, the mask will be placed on your face and secured to the table. You’ll be able to see and breath comfortably at all times.
- Imaging: Images will be taken using a computed tomography (CT) scan or an X-ray machine. For clearer images, CT scans sometimes require an intravenous contrast, or dye, to be used. Positron emission tomography (PET) scan or magnetic resonance imaging (MRI) might also be used. All scans take about four hours.
- Skin markings/Tattoos: To ensure you’re correctly positioned on the table each treatment, your provider will mark the treatment area on the mask or your skin with either a bright, temporary paint or a set of small, permanent tattoos no larger than the head of a pin. Talk with your doctor if you have concerns about tattoos.
- Treatment planning: Your treatment team will use the images taken during your simulation to plan the dose of your radiation, as well as the angles and shapes of radiation beams. The goal is to maximize the dose to the cancer and minimize the dose to normal tissues. It generally takes five to seven days from the time of your simulation until your first treatment.
- Treatment scheduling: Radiation treatments are typically scheduled five days a week, Monday through Friday, over six to seven weeks. The number of radiation treatments depends on the cancer, treatment regimen and goals, and your overall health. Chemotherapy and radiation treatments can be given on the same day.
- Set-up procedure: You’ll have a one-hour set-up procedure before your first treatment. Talk to your provider about taking any pain or anxiety medication that was helpful during your simulation. Therapists will position you on the table as they did during your simulation.
During Treatment
What to expect
Inside the treatment room, your therapist positions your mask and body on the table to ensure you’re in the exact same position every day. Once they leave the room, treatment will start. Radiation is targeted at your tumor and sessions are painless, like getting an X-ray.
Your therapist might move the machine or table to better target the tumor. You will be closely monitored, and you can speak to your provider through a microphone. While the time in the treatment rooms varies depending on the type of radiation, it typically takes 20 to 30 minutes and most of that time is spent positioning you.
Your radiation oncologist and nurse will see you weekly to track your treatment, monitor side effects and address your concerns. Your provider might change your treatment plan based on how you’re responding.
Side effects
While radiation therapy doesn’t hurt when it’s given, some of the side effects cause pain and affect your quality of life. Some side effects last a few days; others can last weeks, months or longer. To speak with a staff member at the Evaluations and Treatment Center about your symptoms, call 626-218-5200.
Below are possible side effects:
Changes to the mouth and throat
- Pain or sores in the mouth and throat
- Dry mouth or thickened saliva
- Pain or difficulty swallowing
- Changes in taste
To help relieve symptoms:
- Brush your teeth with mild toothpaste containing fluoride and a soft-bristle or baby’s toothbrush.
- Remove and clean dentures, bridges or dental prosthesis each time you clean your mouth.
- Use a mouthwash without alcohol or sugar (Biotene or Dentek).
- Use a lip moisturizer (Aquaphor). Don’t use four hours before treatment.
- Rinse your mouth with water or a solution for 15 to 30 seconds every four to six hours or as needed.
- Try mouth moisturizers.
- Sip water or other liquids (coconut water, almond milk, Gatorade, broth) throughout the day.
- Use an aerosol pump spray bottle to moisten your mouth often.
- Use a humidifier, especially at night.
- Avoid air conditioning.
- Use any of these solutions:
- 4 cups of water mixed with 1 teaspoon of salt and 1 teaspoon of baking soda
- One quart of water mixed with 1 teaspoon of salt
- One quart of water mixed with 1 teaspoon of baking soda
Changes inside the nose
- Dryness
- Stuffiness
- Occasional minor nosebleeds
To help relieve these symptoms, keep the inside of your nose moist using saline nose spray or a humidifier.
Ear pain
Radiation can cause swelling or hardening of ear wax. Tell your doctor or nurse if you develop ear pain as the pain may be a sign of infection.
Voice changes
Swelling from radiation can cause hoarseness. To help relieve these symptoms:
- Rest your voice.
- Don’t whisper as it can strain your vocal cords.
- Use a humidifier.
- Gargle with solutions mentioned above.
Skin reactions
Your skin around the treatment area will change, including appearing:
- Pink or tanned
- Bright red or very dark
- Dry, itchy, flaky
Tell your provider if you develop a rash as it might be a sign of infection. Sensitive areas — behind ears and near the collarbone — might blister and peel. Your provider can help treat these areas.
To help relieve symptoms:
- Keep your skin clean: Bathe or shower daily using warm water and gently clean your skin with a mild, unscented soap (Neutrogena, Dove, baby soap, Basis, Cetaphil).
- Use a daily moisturizer: Miaderm lotion is available at City of Hope's Positive Image CenterSM and on Amazon.com.
If your skin is irritated, wear loose-fitting, cotton clothing over the treated area and avoid:
- Makeup
- Perfumes
- Powders
- Aftershave
- Shaving
- Extremely hot or cold temperatures (hot tubs, heating pads, ice packs)
- Scratching your skin
- Tanning
Hair loss
You might lose some or all of the hair on your face, neck or scalp in the area being treated. Hair will usually grow back two to four months after completing treatment.
Difficulty eating and drinking
Radiation to the head and neck can affect your ability to eat enough food to maintain weight and energy level. To maintaining proper nutrition, eat a well-balanced diet high in calories and protein and take a daily multivitamin. Talk to your provider about the best foods and liquids for you.
What to eat and drink based on your symptoms:
Difficulty swallowing
- Eat soft, moist, bland foods taken in small bites and chewed well.
- Use sauces and gravies to soften food.
- Blend or purée your food.
- Speak with your provider about nutritional supplements.
Avoid:
- Very hot foods and liquids
- Dry, hard and coarse foods (e.g., chips, pretzels, crackers, raw vegetables)
- Spices
- Acidic fruits and juices
- Alcohol
- Tobacco
Dry mouth
- Rinse your mouth before eating.
- Add gravies and sauces to food.
- Drink while eating dry foods.
Loss of appetite
- Eat small, frequent meals throughout the day.
- Choose foods and drinks high in calories and protein.
- Eat your meals in a calm place and take your time.
- Eat with family or friends.
- Bring snacks and drinks to treatment.
- Speak with your provider about nutritional supplements.
Nausea
- Eat foods at room temperature or cooler (yogurt, sherbet).
- Cooled or chilled liquids (ginger ale)
- Dry, starchy foods (toast, soda crackers, dry cereal, pretzels)
- Cold chicken or turkey, baked or broiled, with the skin removed
- Soft fruits, vegetables
Avoid:
- Hot foods with strong odors
- Spicy, fatty, greasy, fried foods
- Very sweet foods
- Acidic or citrus foods and juices
- Alcohol
Fatigue
The emotional, mental and physical stress from cancer and its treatment often causes fatigue. Those receiving chemotherapy and radiation simultaneously will feel very fatigued during the last few weeks of treatment. Most patients feel fatigue after a few weeks of treatment. This feeling will slowly subside after you finish treatment but can last for several months post-treatment.
Tips to help manage your fatigue:
- Shift or cut back on your work schedule.
- Plan activities during times you’ll have the most energy.
- Plan naps and time to rest.
- Ask family and friends for help.
- Exercise if that improves your energy.
- Eat foods high in protein and calories.
Sexual health
During treatment, you don’t have to change your sexual activity unless your doctor tells you otherwise. Cancer and its treatment can have severe impacts on your body and sexuality. Talk to your provider about available resources.
Emotional health
The diagnosis and treatment of cancer can be stressful and overwhelming, having a serious effect on your body and mind. Talk to your provider about resources to help your emotional well-being.
Call your doctor if you’re experiencing:
- A temperature of 100.4° F (38° C) or higher
- Nausea, vomiting or both so severe you can’t keep anything down you eat or drink (or take through your feeding tube) for 24 hours
- Constipation not relieved by medication
- Pain not relieved by medication
- Blisters on your skin in the area being treated
If you experience difficulty breathing or any other serious medical issues, call 911.
For urgent care issues, after clinic hours, please call a staff member at the Evaluations and Treatment Center (ETC) at (626) 218-5200.
After Treatment
You’ll have a series of follow-up appointments so your providers can evaluate your response and address any questions. Take care of yourself after treatment ends. Remember:
- While many treatment side effects will slowly go away four to eight weeks after treatment is completed, some might persist longer.
- Take care of your mouth for the rest of your life:
- Have consistent dental follow-up appointments.
- Continue to use the fluoride toothpaste.
- Avoid sweet, sticky foods as they can increase your risk of cavities.
- Avoid tanning or burning your skin. Use a PABA-free sunblock with an SPF of 30 or higher and cover the skin that was treated with radiation.
- Maintain a healthy, well-balanced diet and take a daily multivitamin.
- Avoid alcohol and tobacco.
Follow-up
You’ll have a series of follow-up examinations after your treatment to ensure therapy is successful, detect recurrent cancer and treat side effects of radiation. If your cancer treatment is successful, there’s a low risk — about 2 to 3 percent per year — of developing an unrelated head and neck cancer.
Follow-up visits are typically as follows:
- First year: Every three to four months
- Second year: Every four to six months
- Third to fifth year: Every six months
- Annually thereafter