Lung Cancer
City of Hope takes a team-based approach to your health and offers access to advanced procedures that are not available at other centers. Our thoracic specialists are among the best when it comes to minimally invasive, lung-sparing surgery for lung cancer, and we perform one of the largest volumes of thoracic surgeries in California. We were also the first in our region to offer access to the robotic-assisted endoscopic Monarch platform, which safely and reliably diagnoses patients with small, peripheral nodules in the lung.
Around 240,000 new cases of lung cancer will be diagnosed in the United States this year, mostly among smokers. A growing number of cases are being found in people who never smoked, which means factors like the environment or genetics may be involved.
To accurately diagnose lung cancer, City of Hope uses a combination of leading-edge screening methods and a team of doctors solely focused on treating lung cancer. Our team of thoracic specialists combines its deep expertise with advanced technology.
Lung cancer is a disease whose treatments change rapidly. Your team at City of Hope combines leading-edge technologies — like minimally invasive, laparoscopic and robotic surgery — with the latest targeted therapy, immunotherapy and radiological advances.
Getting lung cancer treatment at City of Hope means you are steps away from labs developing exciting new therapies for lung cancer every day. As a result, the latest and award-winning lung cancer research we conduct moves quickly from the lab to our patients' bedsides.
Getting lung cancer is frightening and devastating. Getting through it and figuring out how to live a long life takes layers of support. At City of Hope, you get access to a strong support network, including staff to help you and your family at every step in your lung cancer journey.
Patient Stories




City of Hope is a nationally recognized leader in the research and treatment of lung cancer. We are one of the few facilities designated as a comprehensive cancer center by the National Cancer Institute.
Our Commitment to Providing the Best Care Includes:
- Lung experts who regularly treat aggressive and late-stage cancer, including complicated cases other institutions may have deemed untreatable
- Cost-effective, low-dose computed tomography scanning technology that can detect cancer earlier and help save lives
- Robotic-assisted endoscopy technology, enables bronchoscopic visualization and lung cancer diagnosis at Stage 1 or 2, which results in safer, quicker and more accurate diagnosis.
- Minimally invasive techniques, such as sputum cytology, needle biopsy, bronchoscopy, endobronchial ultrasound, electromagnetic navigation bronchoscopy, pulmonary function testing, thoracentesis, cervical mediastinoscopy and thoracoscopy
- Our Interventional Pulmonology Program provides the most advanced diagnostic and therapeutic interventions available, including rigid bronchoscopy, medical pleuroscopy and robot-assisted bronchoscopy.
- Investigational diagnostic testing, not yet available to the general public, is offered through enrollment in our clinical trials.
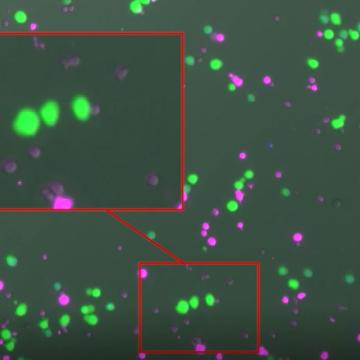
- Precision medicine, such as targeted therapy, CAR T cell therapy and immunotherapy
- Molecular and genetic tests tailor treatment to each patient
- Exceptional supportive care services and survivorship resources
- Smoking Cessation Program designed to help patients successfully stop smoking through medications, behavioral strategies, strategic problem solving and social support

Our collaborative approach, combined with our dedication to advancing cancer care, results in superior lung cancer survival outcomes compared to SEER LA data, making us one of the best choices for lung cancer treatment in the region.

Our developments in the areas of breakthrough cancer drugs, bone marrow transplants and CAR T cell therapy are recognized internationally.
Our leadership in research and innovation continually enhances our ability to provide novel and differentiated approaches to cancer care.
If you or someone you love has been diagnosed with lung cancer, City of Hope has developed an interactive tool to to help you navigate your journey.

Stacy W. Gray, M.D., is deputy director of the Center for Precision Medicine and professor and chief of the Division of Clinical Cancer Genomics within the Department of Medical Oncology & Therapeutics Research, and a secondary appointment in the Department of Population Sciences.
Jae Y. Kim, M.D., is the chief of the Division of Thoracic Surgery and an associate professor in the Department of Surgery. Dr. Kim specializes in esophageal cancer and lung cancer, robotic surgery, mesothelioma and thymoma.

Erminia Massarelli, M.D., Ph.D., M.S., is the co-director of the Lung Cancer and Thoracic Oncology Program, and an associate professor in the Department of Medical Oncology & Therapeutics Research at City of Hope. She specializes in lung and head and neck cancers.
Farhad Mazdisnian, M.D., is Chief of the Division of Pulmonary and Critical Care Medicine in the Department of Medicine at City of Hope.
Loretta Erhunmwunsee, M.D., is a thoracic surgeon and an associate professor in City of Hope's Division of Thoracic Surgery. She sees patients with lung, esophageal and mediastinal tumors. Her research focuses on eliminating health inequity in thoracic oncology patients.
Jae Y. Kim, M.D., is the chief of the Division of Thoracic Surgery and an associate professor in the Department of Surgery. Dr. Kim specializes in esophageal cancer and lung cancer, robotic surgery, mesothelioma and thymoma.

Dan Raz, M.D., M.A.S., is co-director of the Lung Cancer and Thoracic Oncology Program and an associate professor in the Division of Thoracic Surgery. Dr. Raz specializes in esophageal and lung cancer surgery – and in raising public awareness about cancer risks.

Edward S. Kim, M.D., M.B.A., is the physician-in-chief of City of Hope Orange County, vice physician-in-chief of City of Hope National Medical Center, Professor, of the Department of Medical Oncology & Therapeutics Research, and Physician-in-Chief Chair of the Construction Industries Alliance City

In her capacity as director of thoracic medical oncology at the City of Hope Orange County, Jyoti Malhotra, M.D., M.P.H., is excited about offering patients an expansive slate of early-phase clinical trials, to offer more people access to new therapies.

Hugh Davis, M.D., is an assistant clinical professor, Division of Pulmonary and Critical Care Medicine within the Department of Medicine at City of Hope, Duarte, California.
Aria Hong, M.D., is an assistant clinical professor, Division of Hospital Medicine, Department of Medicine.
Arya Amini, M.D., is a radiation oncologist and associate professor in the Department of Radiation Oncology at City of Hope.

Ji Hyun Kim, M.D., is a radiation oncologist at City of Hope's South Bay site.
William D. Boswell Jr., M.D., professor in the Department of Diagnostic Radiology, is an authority in urologic cancers, hematologic malignancies, oncologic imaging, telemedicine and telehealth at City of Hope, as well as a health care leader for Los Angeles County.
Betty Ferrell, Ph.D., M.S.N., R.N., CHPN, FAAN, FPCN, director, Division of Nursing Research and Education, focuses her clinical expertise and research in pain management, quality of life and palliative care.

Virginia Sun, Ph.D., M.S.N., R.N., professor in the Department of Population Sciences, focuses her research on developing and testing interventions to improve patient and family-centered care and surgical outcomes.

Stacy W. Gray, M.D., is deputy director of the Center for Precision Medicine and professor and chief of the Division of Clinical Cancer Genomics within the Department of Medical Oncology & Therapeutics Research, and a secondary appointment in the Department of Population Sciences.
Leonidas Arvanitis, M.D., is a neuropathologist and associate clinical professor in the Department of Pathology.

Massimo D'Apuzzo, M.D., is a neuropathologist and anatomic pathologist focusing on brain tumors.
Linda Malkas, Ph.D., is a professor in the Department of Molecular Diagnostics & Experimental Therapeutics at Beckman Research Institute of City of Hope.

Timothy O'Connor, Ph.D., is Professor Emeritus, Department of Cancer Biology and Molecular Medicine at the Beckman Research Institute of City of Hope, conducting research focusing on DNA repair.