Melanoma Facts
Melanocytes are the pigment-producing cells in your body. While most reside on your skin, they can also be found in your eyes, lips, nailbeds and internal organs. Melanoma originates in melanocytes. Early detection is critical, as survival rates worsen with later detection. The five-year survival rate for Stage 1 melanoma is 98%, for Stage 3 melanoma is 63% and for Stage 4 is 17%.
What are the subtypes?
Four main melanoma subtypes are:
- Superficial spreading melanoma — the most common type — accounts for 70% of all diagnoses, especially for those under age 40.
- Nodular melanoma — the second most common type, comprising 15% of all cases — is aggressive because it grows faster than the other subtypes. It frequently appears in people with light complexions and over age 65.
- Acral lentiginous melanoma is a rare type of melanoma that most diagnosed in people of color. The usual sign is a brown or black skin discoloration, like a bruise or stain, on the sole of your foot or the palm of your hand that grows larger over time.
- Lentigo maligna (early stage) and lentigo maligna melanoma (later stage) account for 4-15% of all cases. They manifest on the face, ears or neck and cause blotchiness. They occur most frequently in elderly people with sun-damaged skin.
Some extremely uncommon subtypes include:
- Spitzoid melanoma can be misdiagnosed as a benign skin mole called a Spitz nevus.
- The dome-shaped Nevoid melanoma ranges in color (brown, black, blue or red) and can also be confused with a benign skin mole.
- Desmoplastic melanoma is rare, comprising four percent of all diagnoses. The usual sign of desmoplastic melanoma is a scar-like texture and appearance in any color but typically pink or red. It tends to manifest on the face, scalp, neck, and sun-exposed parts of the arms and legs.
- Uveal melanoma or ocular melanoma appears in the eyes.
- Mucosal melanoma develops in the membranes lining the eyes, sinuses, anus and vagina.
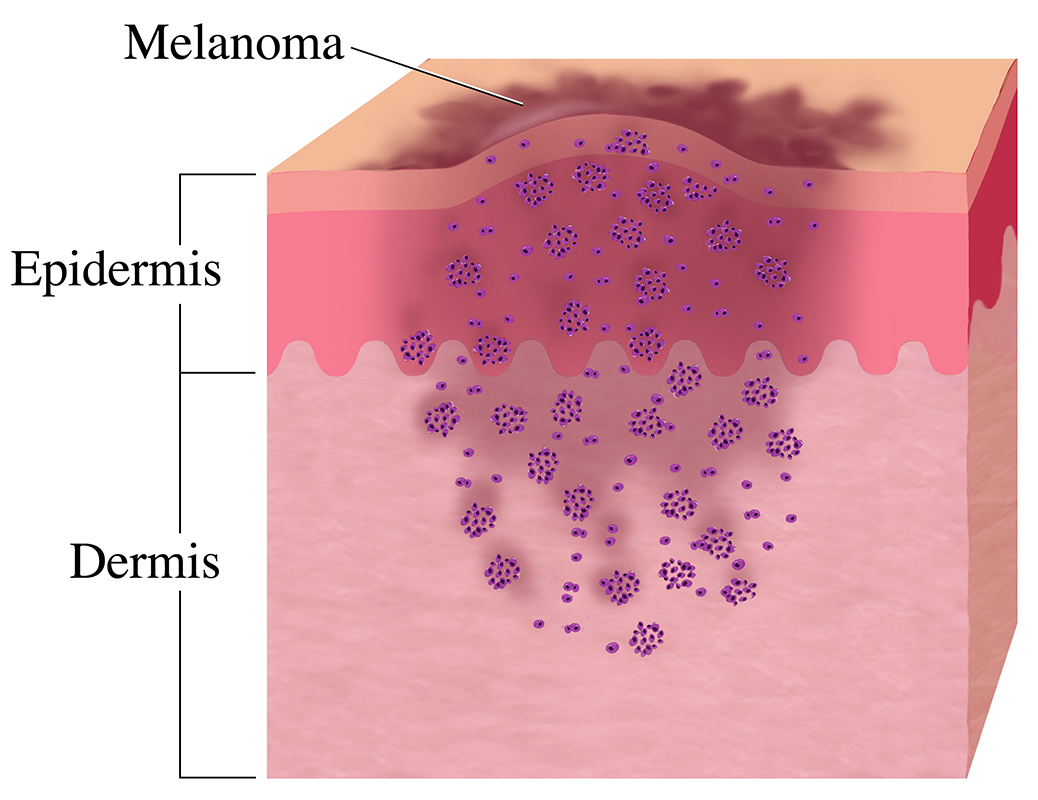
Several factors contribute to the development of melanoma. While the precise cause is likely multifactorial, genetics and sun exposure play significant roles; the latter can induce DNA mutations within melanocytes and other skin cells. When specific cancer-causing mutations develop within melanocytes, the cells in your skin grow uncontrollably and can spread to other parts of your body.

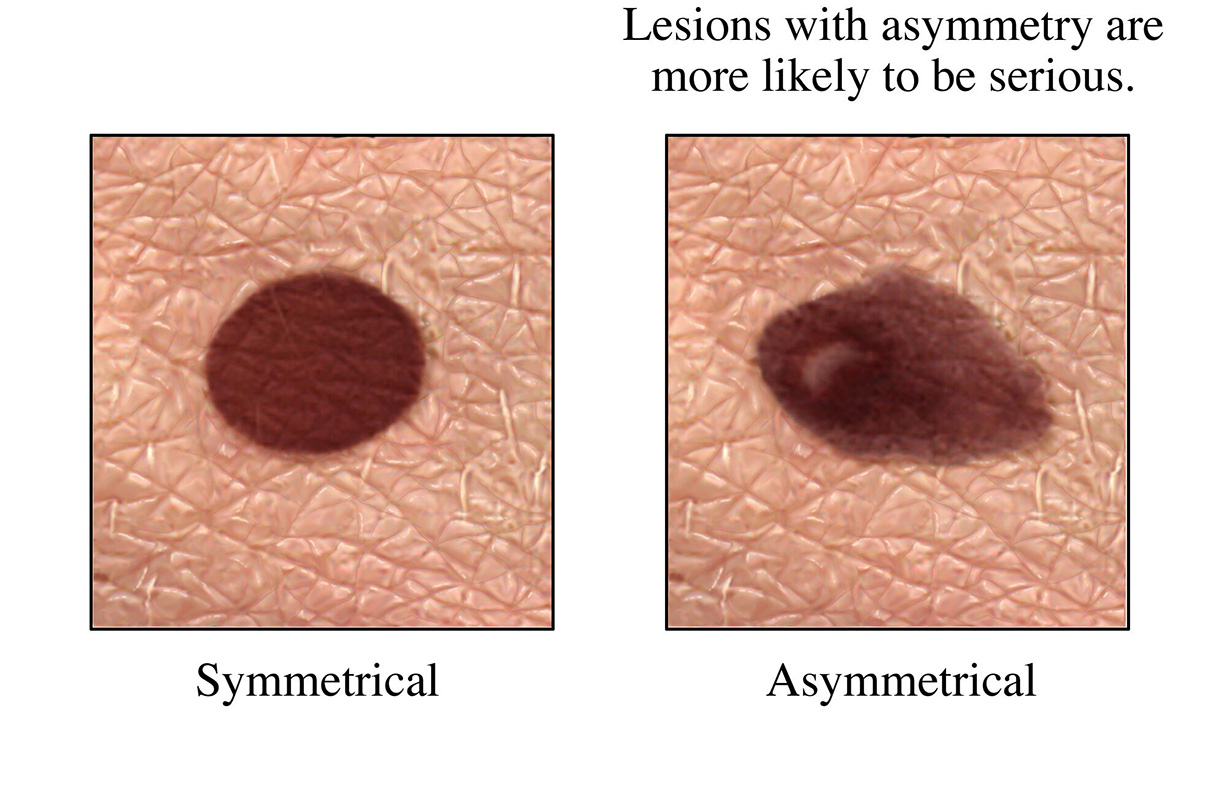
Melanoma commonly manifests as an unusual or atypical mole that appears to be growing or changing. Melanoma can arise from a pre-existing mole, or it can develop de novo from normal skin without moles. The most important clinical symptom to watch out for is any change to your skin. Additional characteristics can include spots with:
- Irregular edges or uneven borders
- Having more than one color
- Asymmetry
- Itchiness
- Oozing, bleeding or ulceration
If you notice any of these skin changes, contact your doctor.
After the physical exam and initial diagnostics and imaging, your doctor assigns a stage that describes how advanced or widespread the melanoma is in your body. Correctly identifying the stage of your melanoma is key to determining the best treatment for you. The stage of the melanoma is based on whether the tumor has spread beyond the primary site. But the cancer progresses, the tumor grows larger and more deeply into the skin layers.
Four Stages of Melanoma
Stages 1 to 2
Tumors are contained within the top layers of the skin.
Stage 3
The melanoma has either spread to the nearby lymph nodes or it has spread beyond the primary tumor without reaching the nearest lymph nodes.
Stage 4
This is the most advanced stage of melanoma in which the tumor has reached beyond the skin and nearby lymph nodes and into distant organs like the liver, lungs, brain, bone or gastrointestinal tract. Stage 4 can also be recurrent melanoma or melanoma that has come back after treatment.
The main risk factor for developing melanoma is exposure to ultraviolet radiation from:
- Natural sunlight
- Tanning beds
- Sun lamps
Other factors that may contribute to developing melanoma include:
- Having many, or unusual, moles
- Having a history of severe, blistering sunburns
- Family history of atypical nevus syndrome (unusual moles) or melanoma
- Having gene changes linked to melanoma
- Exposure to large amounts of toxic substances, such as paraffin oil, coal tar and arsenic compounds
- Being a blond or redhead
- Having light-colored, blue or green eyes
- Having fair skin that easily freckles or sunburns
- Having a weakened immune system
- Having a rare inherited condition called xeroderma pigmentosum
People with darker complexions have a much lower risk of most types of skin cancer, but when they do develop melanoma, they’re much more likely to have rare types, such as acral lentiginous melanoma, an aggressive type affecting the palms of the hands, soles of the feet and nail beds. Melanoma can also develop in the membranes of the mouth, gastrointestinal tract and female genital tract.

Ultraviolet damage is cumulative, meaning it begins building up in your childhood, so prevention should start at a young age. The best ways to lower your risk for skin cancer include shielding the skin as much as possible from UV radiation:
- Use sunscreen and reapply at least every two hours
- Wear protective clothing, including fabrics not easily penetrated by UV light
- Wear other protective items such as hats and sunglasses
- Stay in the shade during peak hours when the sun’s UV rays are most intense (from 10 a.m. to 4 p.m.)
- Avoid tanning salons