Adolfo Garcia-Ocana Lab
Conventional treatment diabetes often relies on insulin injections. Unfortunately, hypo-glycemia (abnormally low blood sugar) and hyperglycemia (high blood glucose) may frequently occur and result in severe secondary complications. Diabetes is associated with progressive loss of functional pancreatic beta cells. In autoimmune type 1 diabetes (T1D), immune self-tolerance is lost leading to the destruction of pancreatic beta cells. Therapies that simultaneously enhance immune tolerance and pancreatic beta cell regeneration and protection could provide a more effective approach for treating T1D.
The pancreatic beta cell adapts to overnutrition by increasing its mass and function. This adaptation is driven by signals derived from nutrient metabolism, growth factors and hormones. Failure to expand in response to metabolic stress leads results in beta cell dysfunction, de-differentiation, death, and development of type 2 diabetes (T2D). Understanding the molecular mechanisms that regulate these cellular processes is critical to the development of new T2D treatments.
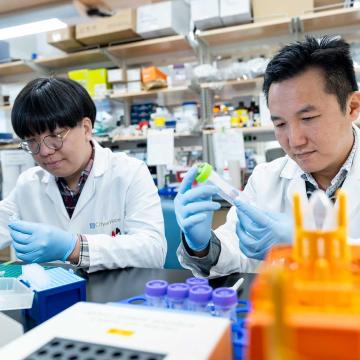
The research in the lab focuses on developing innovative and effective therapies to enhance pancreatic beta cell preservation, pancreatic beta cell function, immune tolerance, and pancreatic beta cell regeneration to manage and treat diabetes.
Adolfo Garcia-Ocaña, Ph.D., is professor and chair of the Department of Molecular & Cellular Endocrinology and the Ruth B. & Robert K. Lanman Endowed Chair in Gene Regulation & Drug Discovery Research.
- Jungeun Lee, volunteer undergraduate student
- Nethravathi Guthalu Puttaraju, B.S., volunteer
Research in the Garcia-Ocana lab focuses on the four listed below:
Project 1: Pancreatic beta cell regeneration
Through collaborations with Sarah Stanley, M.B.B.Ch., Ph.D., Andrew Stewart, M.D., and Robert DeVita, Ph.D. at Icahn School of Medicine at Mount Sinai School of Medicine in New York City, we have found that the combination of the DYRK1A inhibitor, harmine, with widely clinically used GLP-1 receptor (GLP-1R) agonists significantly increases human beta cell mass in vivo in mice transplanted with human islets. This is the first demonstration that a drug or drug combination is capable of specifically expanding human beta cells in vivo. For these studies we have used the latest 3D imaging and tissue clarifications techniques (iDISCO), mice with human islets transplanted under the kidney capsule and drug delivery using minipumps for several months. These studies are funded by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (NIH/NIDDK)and the Juvenile Diabetes Research Foundation
Project 2: Combination therapy to reverse type 1 diabetes
This project analyzes in vivo the therapeutic capacity of a combination therapy with DYRK1A inhibitors, GLP-1R agonists and an anti-CD3 antibody to reverse early onset T1D in NOD mice. These studies will be extended to mice with established T1D. These studies are funded by NIH/NIDDK.
Project 3: Myc as a master regulator of beta cell growth and function
The transcription factor, Myc, is a master regulator of adaptive beta cell expansion in situations of overnutrition and obesity. This action is impaired in aging by epigenetic changes that diminish its binding capacity to DNA. However, whether Myc contributes to the regulation of beta cell function is unknown. This is being explored through new research funded by NIH/NIDDK.
Project 4: Single cell omics of human islet cells
Single-nucleus RNA sequencing (snRNA-seq) has compatibility with frozen samples, elimination of dissociation-induced transcriptional stress responses, and affords enhanced information from intronic sequences that can be leveraged to identify pre-mRNA transcripts. By performing snRNA-seq analysis of human islets in vitro and in vivo in immunodeficient mice transplanted with human islets, we found that new, non-canonical gene sets more accurately identify endocrine cell types in the snRNA-seq analysis; and three different β-cell subpopulations reflect differences in their INS mRNA transcriptional stage and distinct biological functions according to gene set enrichment analysis. Overall, our studies support the use of snRNA-seq and pre-mRNA analysis as a tool for deciphering human islet cell populations and subpopulations and their distinct biological functions in health and disease.
The knowledge obtained from these studies may lead to the development of effective and innovative new therapies to treat diabetes in the future.
To view all lab publications, please click the link below: